The Benefits of Radiofrequency Ablation for Chronic Back Pain
Chronic back pain can be a real drag, making everyday activities challenging. But there's good news! Radiofrequency ablation, a cool medical procedure, is the answer to relieving that nagging pain.
This treatment uses special radio waves to target and calm down those pesky nerves causing the pain. It's like hitting a mute button on your back pain! This article deals with the benefits of radiofrequency ablation for chronic back pain. Let's dive into how this amazing technique can bring back the joy in your daily life.
Understanding Chronic Back Pain
Before exploring RFA, it's crucial to understand what chronic back pain is and why it's such a complex issue to address.
Chronic back pain is defined as pain that persists for 12 weeks or longer, even after an initial injury or underlying cause of acute back pain has been treated. The causes are multifaceted, ranging from degenerative disc disease, herniated discs, to spinal stenosis and arthritis.
This pain not only limits mobility but also affects an individual's mental health, contributing to a cycle of pain that's hard to break.
Living with chronic back pain can be debilitating. It restricts one’s ability to perform simple daily tasks, engage in physical activities, and can even impair one's work life, leading to significant lifestyle changes and sometimes, disability.
Traditionally, chronic back pain treatments include medication, physical therapy, and in severe cases, surgery. However, these approaches often have limitations:
- Medications can lead to dependency and have side effects.
- Physical therapy requires a long-term commitment and doesn't always yield pain-free results.
- Surgery carries significant risks and requires extensive recovery time.
Given these limitations, the search for effective, minimally invasive treatments has led to the development and adoption of Radiofrequency Ablation.
Introduction to Radiofrequency Ablation
Radiofrequency Ablation is a minimally invasive procedure that uses heat generated from radio waves to target specific nerves that are transmitting pain signals to the brain. By carefully destroying these nerve fibers, RFA can significantly reduce or even eliminate pain in the treated area. Below is how RFA works:

- Patient Evaluation: Not everyone is a candidate for RFA. A thorough evaluation, including medical history, physical examination, and sometimes diagnostic nerve blocks, is performed to identify the source of pain.
- The Procedure: Using a local anesthetic and sedation, a needle is inserted into the targeted area guided by imaging techniques like fluoroscopy. Once in place, a radiofrequency current is passed through the needle, heating up the nerve and disrupting its ability to send pain signals.
- Post-Procedure Care: Recovery is quick, with most patients returning to normal activities within a few days. The full effect of the pain relief usually becomes apparent in about two weeks.
Advantages of RFA
RFA offers several benefits over traditional treatments:
- Minimally Invasive: With no need for incisions, the risk of complications and recovery time are significantly reduced.
- Effective Pain Relief: Many patients experience substantial pain relief that can last from six months to several years.
- Improved Quality of Life: With pain management under control, patients can return to daily activities and enjoy a better quality of life.
The Science Behind RFA
Radiofrequency Ablation (RFA) is a sophisticated pain management technique that offers a promising solution for patients suffering from chronic pain, particularly in cases where conventional therapies have failed to provide relief.
This procedure leverages the power of radiofrequency energy to disrupt pain signaling pathways, offering a unique approach to pain management.
How RFA Works at a Cellular Level
RFA works by delivering high-frequency radio waves through a needle inserted into the targeted tissue. The tip of the needle emits radiofrequency energy, which produces heat. When this heat is applied to a specific nerve tissue, it causes a thermal lesion or burn, effectively disrupting the nerve’s ability to transmit pain signals to the brain.
At the cellular level, this process involves the denaturation of proteins within the nerve cells, leading to a cessation of nerve conductivity. This disruption doesn't destroy the nerve completely but alters its signaling ability, providing pain relief without significant loss of other sensations.
Targeting Nerve Tissues Responsible for Pain Signals
Precision is key in RFA. The procedure targets nerves known to carry pain signals from the specific area being treated. Before the ablation is performed, diagnostic nerve blocks may be used to identify the precise nerve or nerve group responsible for the pain.
Imaging techniques such as fluoroscopy (live X-ray) or ultrasound help guide the needle to the exact location, ensuring the radiofrequency energy is applied only to the intended nerve tissues. This targeted approach minimizes damage to surrounding tissues and maximizes the efficacy of the treatment.
Comparison with Other Pain Management Technologies
RFA stands out among pain management technologies for several reasons:
- Invasiveness and Recovery Time: Compared to surgical interventions, RFA is minimally invasive, requiring only a needle puncture. This results in shorter recovery times and less risk of complications.
- Duration of Relief: While injections or nerve blocks provide temporary relief, RFA offers a longer-lasting solution. The effects of RFA can last from six months to over a year, and the procedure can be repeated if necessary.
- Effectiveness: RFA has been shown to be particularly effective for certain conditions such as facet joint pain, sacroiliac joint pain, and some types of nerve pain, offering significant relief when other treatments have not been successful.
- Safety Profile: The risk of infection, bleeding, or significant nerve damage is considerably lower with RFA compared to surgical procedures. The side effects are generally mild and temporary.
Compared to other non-surgical treatments like physical therapy, medications, or corticosteroid injections, RFA provides a more durable solution to pain management without the side effects associated with long-term medication use or the temporary nature of injections.
Benefits of Radiofrequency Ablation for Chronic Back Pain
Radiofrequency Ablation (RFA) is increasingly recognized as a valuable treatment for chronic back pain, offering many benefits ranging from significant pain reduction to improved functionality and quality of life.
This minimally invasive procedure has shown promising results in various studies and personal accounts, highlighting its effectiveness and safety. Below, we explore the multifaceted benefits of RFA for individuals suffering from chronic back pain.

- Effectiveness in Reducing Pain
Numerous studies have validated the efficacy of RFA in managing chronic back pain. Research by Van Wijk et al. that up to 70-80% of patients experience substantial pain relief following the procedure. These high success rates underline RFA's role as a critical option for patients who have not found relief through conventional treatments.
Personal accounts from patients who have undergone RFA often reflect significant improvements in pain levels and quality of life. Many describe returning to activities they thought were a part of their past, such as hiking, biking, or simply engaging in daily tasks without the hindrance of pain.
- Minimally Invasive Nature
RFA is performed using a needle electrode, guided by imaging techniques to target specific nerves. Because it does not require large incisions or general anesthesia, patients usually experience minimal downtime.
Most can return to their normal activities within a few days, making RFA an attractive option for those seeking an alternative to more invasive surgical procedures.
The safety profile of RFA is exceptionally favorable, especially when compared to surgical options. The risks of infection, bleeding, or significant nerve damage are considerably lower. This safety, combined with the procedure's efficacy, makes RFA a compelling choice for managing chronic back pain.
- Long-term Relief
The duration of pain relief following RFA can vary, but many patients report experiencing benefits for six months to over two years. Factors such as the specific condition being treated, the patient's overall health, and adherence to post-procedure recommendations can influence the longevity of results.
- Improvement in Functionality and Quality of Life
RFA can significantly improve mobility and the ability to perform daily activities, contributing to an enhanced quality of life. Patients often report a notable decrease in pain, which allows them to resume hobbies and activities without the constant burden of back pain.
The reduction in chronic pain also has profound psychological benefits, including decreased anxiety and depression, improved sleep patterns, and an overall more positive outlook on life.
- Reduced Need for Pain Medication
One of the most significant benefits of RFA is the potential to reduce or eliminate the need for oral painkillers, including opioids. By addressing the source of pain directly, RFA can decrease the reliance on medications and their associated side effects, including the risk of dependency.
The opioid crisis has highlighted the need for effective pain management strategies that do not rely on medication. RFA offers a viable solution, contributing to efforts aimed at reducing the prevalence of opioid use and dependence among patients with chronic pain.
Ideal Candidates for RFA
The journey to RFA begins with pinpointing those who stand to benefit most from this procedure. Ideal candidates are typically those who have battled chronic back pain for over three months without finding solace in conventional therapies like medications or physical therapy.
The pain must be well-localized, stemming from a source that can be precisely targeted. A successful response to a diagnostic nerve block often preludes the effectiveness of RFA, acting as a litmus test for its potential success.
It's also essential that candidates do not have significant psychological conditions that might influence pain perception, ensuring a clearer path to treatment efficacy.
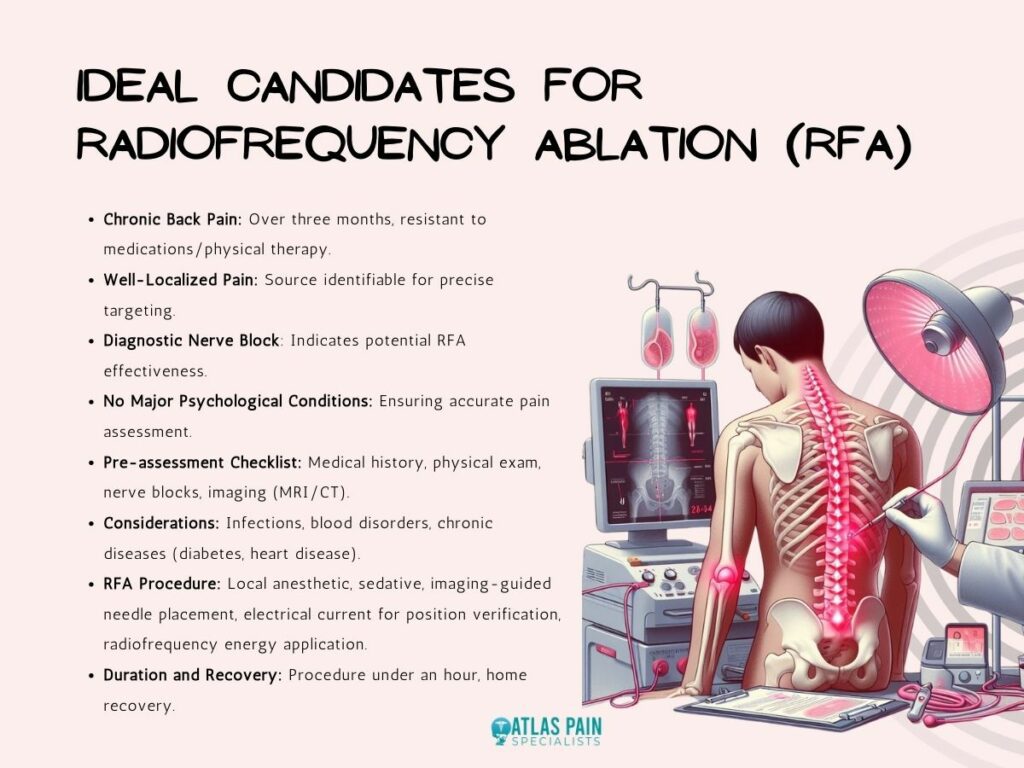
Pre-assessment and Diagnostic Procedures: A Checklist
Before proceeding with RFA, a comprehensive pre-assessment phase ensures the procedure's appropriateness and maximizes its success rate. This includes:
- A thorough medical history review and physical examination to gauge the patient's overall health and specific pain characteristics.
- Diagnostic nerve blocks, which help confirm the pain's origin, ensuring RFA targets the correct nerves.
- Imaging studies, like MRI or CT scans, to provide a clear picture of the anatomical structures involved and any underlying conditions that may be addressed by RFA.
Patients with infections, blood clotting disorders, or chronic conditions such as diabetes or heart disease require careful consideration and preparation before undergoing RFA.
The RFA Procedure Explained
RFA is a marvel of medical technology, offering pain relief through a minimally invasive approach.
- The procedure begins with the patient receiving a local anesthetic and, if necessary, a mild sedative.
- Under imaging guidance, such as fluoroscopy or ultrasound, a needle is precisely positioned near the nerve responsible for the pain.
- A small amount of electrical current is then passed through the needle to ensure its correct placement by stimulating the nerve, minimizing the risk of damage to surrounding areas.
- Once the correct position is confirmed, radiofrequency energy is delivered through the needle, creating heat that disrupts the nerve's pain-transmitting capabilities.
The procedure typically lasts less than an hour, after which the patient can usually return home to begin the recovery process.
Recovery: What to Expect
The recovery timeline and what patients can expect post-RFA include:
- Immediate Post-procedure: Patients may experience some soreness at the injection site, typically subsiding within a few days.
- Pain Relief Timeline: Full pain relief benefits from RFA might take up to three weeks to manifest, with the potential to last from six months to several years.
- Follow-up Care: A follow-up visit is crucial to assess the treatment's outcome and discuss any further necessary steps.
Potential Risks and Side Effects
While Radiofrequency Ablation (RFA) is a relatively safe and effective treatment for chronic back pain, it is not without its potential risks and side effects. Understanding these is crucial for patients to make informed decisions and to know what to expect both during and after the procedure.
Here’s a breakdown of the common and rare complications associated with RFA, along with guidance on managing side effects and when to seek medical help.

Common Side Effects
- Temporary Discomfort: The most common side effect is temporary discomfort at the site of the injection, including tenderness, swelling, or bruising. This usually resolves on its own within a few days.
- Transient Nerve Pain: Some patients may experience an increase in nerve pain or a burning sensation post-procedure, which generally subsides within a few days to a week.
Rare Complications
- Infection: Although rare, there is a risk of infection at the puncture site. This risk is minimized by using sterile techniques during the procedure.
- Bleeding: A small risk of bleeding exists, especially for patients with underlying blood clotting disorders or those on anticoagulant therapy.
- Nerve Damage: There's a slight risk of unintended nerve damage, which could lead to numbness, weakness, or loss of muscle function in the affected area.
- Allergic Reactions: Allergic reactions to the anesthetic used during RFA are possible but uncommon.
Managing Side Effects
Most side effects of RFA are mild and can be managed at home with simple measures such as:
- Applying ice packs to the treatment area to reduce swelling and discomfort.
- Taking over-the-counter pain relievers, as recommended by your healthcare provider, to manage pain.
- Resting the affected area for a day or two, while avoiding strenuous activities until the discomfort subsides.
When to Seek Medical Help
Patients should be vigilant for signs of more severe complications and seek immediate medical attention if they experience:
- Signs of infection, such as fever, increased redness, swelling, or pus discharge from the injection site.
- Severe or persistent pain that does not improve with over-the-counter pain medication.
- Sudden weakness, numbness, or loss of bladder or bowel control, which could indicate nerve damage.
Comparing Risk Profiles
When compared to other treatments for chronic back pain, such as surgery, RFA has a lower risk profile. Surgical interventions often come with a higher risk of complications, including infection, prolonged recovery times, and the potential for failed back surgery syndrome.
In contrast, RFA is a minimally invasive procedure with a quicker recovery time and fewer risks, making it an attractive option for many patients.
About Dr. Sean Ormond